

Breast Cancer Staging: are BI-RADS categories just for screening?
BI-RADS classifications are primarily used for breast cancer screening, and only secondarily for breast cancer staging, if at all. The BI-RADS system was an attempt to reduce the confusion in interpreting breast mammograms and ultrasounds. Essentially, a BI-RADS classifications indicates a radiologist's opinion as to the absence or likelihood of breast cancer. What the BI-RADS classification system ('Breast Imaging Reporting and Data System') indicates is whether or not there are certain aspects of the mammogram findings which are suspicious to highly-suspicious for malignancy. If there are, then a decision is made to take additional imaging studies and/or a biopsy sample. However, it is only through the microscopic evaluation that a diagnosis of breast cancer is either made or ruled out. If the microscopic evaluation confirms that the suspicious anomaly is in fact breast cancer, then the staging process begins in earnest.
BI-RADS categories
| BI-RADS categories | criteria/evidence/action |
| 0 | Need for additional imaging for evaluation. No ability to comment |
| 1 | Negative. Nothing to comment on |
| 2 | Benign finding |
| 3 | Probably benign. short term follow-up recommended. |
| 4 | Suspicious abnormality found. Biopsy might be considered |
| 5 | Highly suggestive of malignancy. Biopsy should be taken |
| 6 | Proven malignancy by a known biopsy. |
Patterns of microcalcifications can suggest malignant breast cancer nearby
Probably the earliest indication of potential breast cancer as viewed on a screening mammogram is the presence of microcalcifications. Most microcalcifications are due to benign causes, but some patterns, such as fine, pleomorphic microcalcifications, would be suspicious for malignancy, probably requiring additional studies and short-term follow-up.

BI-RADS helps interpret mammographic breast density
The BI-RADS classification and reporting system helped to establish a more-standardized 'lexicon' of words used to describe mammographic findings. For example, breast density is described as follows:the breast is almost entirely fat (<25% glandular), shows scattered fibroglandular densities (25-50%), demonstrates heterogeneously dense breast tissue (51-75%), or, the breast is extremely dense (> 75% glandular). Breast density is considered by some to be a mild risk factor for breast cancer development, though having dense breast tissue certainly is not indicative of the presence of breast cancer.
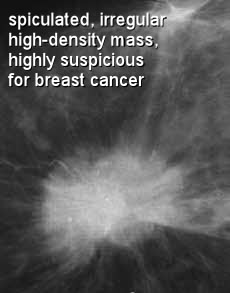
Breast mass characteristics are described, if present
BI-RADS classifications also take into account the 'mass characteristics', which can be more or less suspicious for malignancy. A breast 'mass' is defined as a space occupying lesion seen in two different projections(two different X-ray 'views'). When a potential mass is seen in only one projection it is usually just called a 'density' until a 'three-dimensional' shape can be confirmed. Mass margins are also defined in terms of how 'well circumscribed' they are. Usually mass margins are more suspcious for malignancy when they have poorly defined margins, perhaps indicating that some cells may be 'infiltrating' into the surrounding tissue.
Any archictural distortion of focal asymmetry on the mammogram is reported
BI-RADS reports also consider whether or not the mammogram shows an 'architectural distortion', which means that no mass is visible, but the normal 'view' or structure (architecture) is not what it is supposed to be, but is distorted some how. Sometimes the mammogram might reveal a 'focal asymmetry', which means that there is some sort of increased density, but lacking borders or a distinct shape. In the case of either an architectural distortion or focal asymmetry, the screening physicians will likely perform additional, more detailed breast imaging studies until they find something conclusive. Experienced radiologists can usually have a good 'feel' for whether or not a suspcious mammogram image needs to be biopsied or not.
If the biopsy reveals malignant cells, then a more detailed evaluation and breast cancer staging process is initiated. The original mammograms and any supplemental imaging informing the screening/BI-RADS evaluation may then be used in the staging process. Breast cancer staging is really aimed at learning as much as possible about a particular breast tumor, and this will certainly include any information learned through the screening and BI-RADS classifications, but essentially the BI-RADS classification is a breast cancer screening tool.
The original imaging studies become important frames of reference for monitoring the effectiveness of breast cancer treatments.
However, one of the most important aspects of both the screening mammography itself as well as the BI-RADS classifications, is that it enables the doctors to monitor the effectiveness of treatment. When the same image or view is compared weeks or months into treatment in relation to the original screening images, one can clearly see whether or not a mass or distortion (representing an area of malignant cells growth) is responding to chemotherapy and other treatments. (i.e. they are reduced in size)
BI-RADS 4 and 5 have a certain positive predictive value for breast cancer
The BI-RADS classifications are related to breast cancer staging only in the sense that the higher BI-RADS categories are thought to have a certain Positive Predictive Value,(or PPV) for breast cancer. Remember, though, that breast cancer staging concern the 'extent' of the breast cancer, namely whether or not there is evidence of invasion beyond the breast duct wall, whether breast cancer cells are present in the lymph nodes, and whether or not there is evidence of distant metastasis. For initial breast cancer screening results of BI-RADS category 4 and above, usually it is a biopsy which confirms the presence and/or extent of the local breast cancer. It is possible that additional imaging studies such as MRI and PETscans would be used shortly after an initial mammogram, which may give some indication of the extent of breast cancer spread, if present. But, the main and only goal of breast cancer screening and the BI-RADS categories is to determine whether or not there is a threat of breast cancer, so that if ultimately breast cancer is confirmed, full staging and treatment may begin without delay.
| BI-RADS categories | Approximate Positive Predictive Value for Breast Cancer |
| 0 | 0% |
| 1 | 0% |
| 2 | 0% |
| 3 | 2%-3% |
| 4 | 26%-30% |
| 5 | 90%-97% |
| 6 | 100% |
BI-RADS 3 is very low risk of breast cancer, but one of most 'talked about' classifications.
BI-RADS category 3, or 'probably benign' is perhaps the most controversial of the BI-RADS classifications. A mammogram which a radiologist interprets as BI-RADS category 2, 'probably benign' requiring follow-up exam only, statistically turns out to be the correct interpretation about 97% of the time. That means, a BI-RADS 2 classification has a PPV for breast cancer of 3% or less. Quite often the findings of BI-RADS 2 are either of microcalcifications on the mammogram, or a psuedo-mass on an ultrasound but not seen on mammogram. Even if a developing breast cancer was missed, it would be caught on the follow-up exam, and most of these would be either in-situ (stage 0) or a very small mass (stage 1).
BI-RADS 4 has a 30% predictive value for breast cancer
BI-RADS category 4 has a positive predictive value for confirmed breast cancer of just over 25%-30%, and the usually mammographic finding is of a mass with or without microcalcifications. Most of these turn out to be fibroadenoma or fibrocystic changes. BI-RADS category 5, on the other hand, has a very positive predictive value for breast cancer at nearly 90-97%. So, in that sense, a BI-RADS category 5 classification from a screening mammogram might in fact be considered the first step in a breast cancer staging process.
Overall, BI-RADS is a breast cancer screening procedure
There is no question that breast cancer screening can cause a lot of anxiety for women. If a woman is 'called back' for follow up imaging it can lead to even more anxiety and thoughts such as "oh dear, they are staging me for breast cancer!" This is not the case. There is a chance, however, that a BI-RADS 4 mammogram interpretation will lead to a biopsy, which could statistically has just over a 1 in 4 chance of being breast cancer. A radiologist report indicating a BI-RADS category 5 lesion, on the other hand, has a very high probability (around 95%) of being breast cancer. In this case, the biopsy sample will probably be examined quite thoroughly. (In fact, if it is small enough the entire lesion could be removed surgical as part of the biopsy process.) The pathological/histological evaluation of a biopsy specimen following a BI-RADS 5 mammogram can be considered the start of the breast cancer staging process.
References
- Lazarus, E., Mainiero, MB., Schepps, B., Koelliker, SL., Lvingston, LS., BI-RADS Lexicon for US and Mammography: Interobserver Variability and Positive Predictive Value. Radiology, (May 2006) 239(2): 385 - 391.
- Berg, WA., Breast Imaging Reporting and Data System, Inter- and Intraobserver Variability in Feature Analysis and Final Assessment. Department of Radiology, University of Maryland School of Medicine, 22 S. Greene St., Baltimore, AJR (2000) 174:1769-1777.
- Badgwell BD, Giordano SH, Duan ZZ, Fang S, Bedrosian I, Kuerer HM, et al. Mammography Before Diagnosis Among Women Age 80 Years and Older With Breast Cancer. J Clin Oncol. (Apr 2008)
- Nakahara H, Namba K, Wakamatsu H, Watanabe R, Furusawa H, Shirouzu M, et al. Extension of breast cancer: comparison of CT and MRI. Radiat Med.( Jan-Feb 2002) 20(1):17-23.
- American College of Radiology. ACR Breast Imaging Reporting and Data System (BI-RADS) Web site. Available at www.acr.org.
- Zonderland HM. The role of ultrasound in the diagnosis of breast cancer. Semin Ultrasound CT MR. (Aug 2000);21(4):317-24.
- Marchick J, Henson DE. Correlations between access to mammography and breast cancer stage at diagnosis. Cancer.( Mar 2005)
- Wiratkapun C, Wibulpolprasert B, Lertsithichai P.Breast cancer in patients initially assigned as BI-RADS category 3. J Med Assoc Thai. (Jun 2006) 89(6):834-9.
- Baum JK, Hanna LG, Acharyya S, Mahoney MC, Conant EF, Bassett LW, Pisano ED. Use of BI-RADS 3-Probably Benign Category in the American College of Radiology Imaging Network Digital Mammographic Imaging Screening Trial. Radiology. (Jul 2011) 260(1):61-7.
- Rieber A, Schirrmeister H, Gabelmann A, Nuessle K, Reske S, Kreienberg R, Brambs HJ, Kuehn T. Pre-operative staging of invasive breast cancer with MR mammography and/or PET: boon or bunk? Br J Radiol. (Oct. 2002)75(898):789-98.
- Muttarak, M., Srivichai, K., Chaiwun, B. Sukhamwant, N. The Breast Imaging Reporting and Data System-BI-RADS. Positive Predictive Value. Chiang Mai Med J (2010);49(3):111-116.
- Tan YY, Wee SB, Tan MP, Chong BK. Positive predictive value on BI-RADS categorization in Asian population. Asian J of Surg (2004);27:186-91.
- Orel SG, Kay N, Reynolds C, et al. BI-RADS categorization as a predictor of malignancy. Radiology (1999): 211: 845-850.
Back to breast cancer staging list.
End of page Navigation links: Breast Cancer home or Back to top
Copyright © 1999 - present. Steven B. Halls, MD . 1-780-608-9141 . [email protected]